Pneumocystis Pneumonia (PCP)
What is Pneumocystis pneumonia?
- Pneumocystis pneumonia (PCP), a severe, infectious lung disease, was recognized just after World War II in Europe when it killed malnourished, premature infants in hospitals.
- Subsequently, occasional cases were identified among immunodeficient patients.
- With the start of the AIDS epidemic, the incidence of PCP increased rapidly, and it is still a common opportunistic infection in AIDS patients who are not receiving preventive care.
Signs and Symptoms of Pneumocystis pneumonia
- Many people are infected with the fungus that causes PCP, but the infection is latent because it is kept under control by the immune system.
- In immunocompromised individuals, however, the organism causes disease.
- The signs and symptoms of Pneumocystis pneumonia typically begin slowly after an incubation period of 4 to 6 weeks, with gradually increasing shortness of breath and rapid breathing.
- Fever is usually slight or absent, and only about half of the patients have a cough, which is non-productive.
- As the disease progresses, a dusky coloration of the skin and mucous membranes appears and gradually gets worse—this is caused by poor oxygenation of the blood that can become fatal.
Causative Agent of Pneumocystis pneumonia
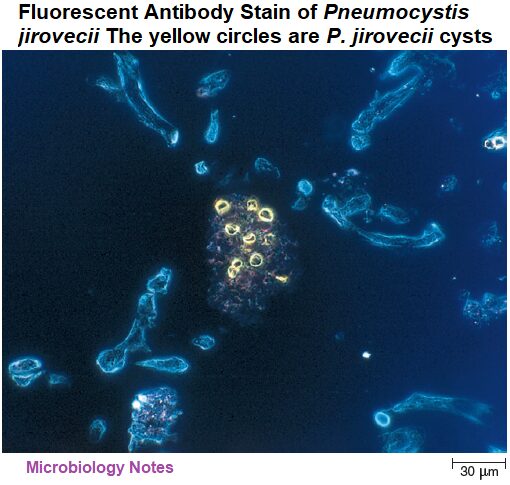
- Pneumocystis pneumonia is caused by Pneumocystis jirovecii, a tiny yeast-like fungus.
- The organism was formerly classified as P. carinii and it is still sometimes known by that name (explaining the acronym PCP for this type of pneumonia).
- P. jirovecii differs from many fungi in the chemical makeup of its cell wall, which makes it resistant to medications often used against fungal pathogens.
- The organism forms cysts that have a characteristic appearance, helping in its identification. It has not reliably been cultivated in vitro.
Pathogenesis of Pneumocystis pneumonia
- P. jirovecii cells are easily inhaled into lung tissue.
- In experimental infections, these attach to the alveolar walls, and the alveoli fill with fluid, macrophages, and masses of P. jirovecii cells in various stages of development.
- Later, the alveolar walls become thickened and scarred, preventing the free passage of O2.
Epidemiology of Pneumocystis pneumonia
- Pneumocystis jirovecii is distributed worldwide.
- Most children are infected with P. jirovecii soon after birth at an early age although the infection is asymptomatic.
- The source and transmission of human infections are unknown.
- Most cases of PCP occur in people with immunodeficiency, but it is uncertain whether their disease is caused by reactivation of a latent infection, or new infection from inhalation of cells.
- Epidemics among hospitalized malnourished infants and elderly nursing home residents suggest airborne spread, and P. jirovecii has been detected in indoor and outdoor air by using polymerase chain reaction (PCR).
Treatment and Prevention of Pneumocystis pneumonia
- PCP is most often treated with co-trimoxazole (TMP-SMX).
- Alternative medications are given to people who cannot tolerate TMP-SMX because of its side effects—mainly rash, nausea, and fever.
- For unknown reasons, people with HIV disease are more likely to develop these side effects than others.
- Oxygen therapy and steroids (to reduce inflammation that worsens symptoms) are also given and can significantly decrease mortality.
- After treatment for PCP, individuals with HIV disease must receive preventive medication indefinitely, or until they have a sustained rise in CD4+ T-cell count to above 200 cells/μL (a CD4+ cell count of 200 cells/μL or lower indicates AIDS).
- To prevent PCP, HIV-infected people are typically started on medication as soon as they become immunodeficient, as indicated by a CD4+ T-cell count below 200 cells/μL, or until development of characteristic opportunistic diseases.
The main features of Pneumocystis pneumonia are presented in table:
| Signs and symptoms | Gradual onset, shortness of breath, rapid breathing, non-productive cough, slight or absent fever, and dusky color of skin and mucous membranes. |
| Incubation period | 4 to 8 weeks |
| Causative agent | Pneumocystis jirovecii (previously known as P. carinii )—a fungus |
| Pathogenesis | Inhaled fungal cells attach to alveolar walls, causing alveoli to fill with fluid, macrophages, and fungal cells. Alveolar walls thicken, impairing O2 exchange. |
| Epidemiology | Most humans become infected in early childhood—source of human infections is unknown. Disease arises in individuals with immunodeficiency such as those with HIV/AIDS; epidemics can occur in hospitalized premature infants and nursing home residents. |
| Treatment and prevention | Treated with antimicrobial medications. Prevented by giving the same medications prophylactically in those with AIDS, when the CD4+ T-cell count drops below 200 cells/μL. |
Reference and Sources
- https://www.encyclopedia.com/medicine/diseases-and-conditions/pathology/acquired-immunodeficiencysyndrome
- https://quizlet.com/134068889/microbiology-chapter-28-flash-cards/
- https://wwwnc.cdc.gov/eid/article/10/10/03-0985_article
- https://quizlet.com/32032692/chapter-28-flash-cards/
- https://quizlet.com/197488327/bio-260-exam-4-flash-cards/
- https://faculty.mtsac.edu/canderson/pathogenic%20properties%20list%20.pdf
- https://quizlet.com/170711555/microbiology-flash-cards/
Also Read:
- Fungal Disease
- Mesothelioma Lung Cancer
- Third Golden Age of Microbiology
- Exposure and Transmission of Infectious Disease
- Gonorrhea: Causative Agent, Symptoms, Treatment and Prevention
- Chlamydia: Introduction, Epidemiology, Transmission, Treatment and Prevention
- Histoplasmosis: Symptoms, Pathogenesis, Treatment and Prevention
- Cold sores : Introduction, Entry, Symptoms, Diagnosis and Cure
- Nosocomial Infection: Introduction, Source, Control and Prevention
- Chickenpox (Varicella) and Shingles (Herpes Zoster)
- Hansen’s Disease: Symptoms, Causative Agent, Pathogenesis and Treatment
