Definition
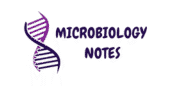
Agglutination is an antigen-antibody reaction in which particulate antigens (e.g., cells, bacteria, or latex beads) clump together in the presence of specific antibodies. This reaction is a visible, rapid, and sensitive method used in diagnostics, blood typing, and microbiology. An agglutination reaction occurs when specific antibodies cross-link cells or particles to form an immune complex.
- Agglutination reactions usually create visible clumps or aggregates, called agglutinates, that the naked eye can see.
- For the diagnosis of certain diseases direct agglutination reaction is very useful.
- For example, the Widal test involves a reaction that agglutinates typhoid bacilli when an individual who has typhoid fever mixes serum containing typhoid antibodies with them.
Uses and application of Agglutination Reaction
- Researchers have also developed techniques that employ microscopic synthetic latex spheres coated with antigens.
- These coated microspheres bind antibodies in a patient’s serum specimen to identify viral disease rapidly when cultures are not feasible (e.g., HIV).
- Researchers also use latex agglutination tests to detect antibodies that develop during certain mycotic (fungal), helminthic (worm), and bacterial infections, as well as in drug testing.
- Researchers can also coat microspheres with monoclonal antibodies to capture antigens from patient specimens.
Hemagglutination Reaction
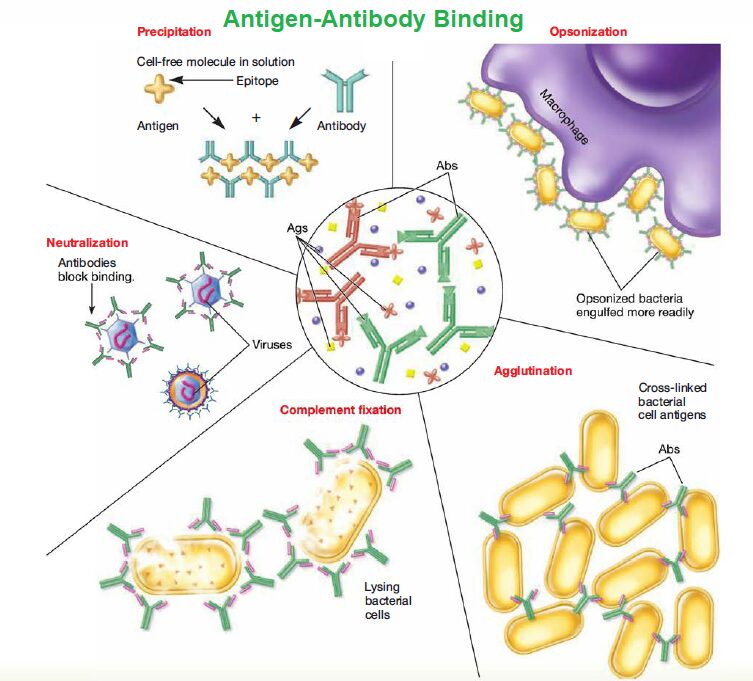
- Antibodies attach to surface antigens, cross-link red blood cells, and result in hemagglutination, which researchers routinely use in blood typing.
- In addition, some viruses can accomplish viral hemagglutination. For example, if a person has a certain viral disease, such as measles, antibodies will be present in the serum to react with the measles virus particles and neutralize them.
- Normally, when researchers mix measles virus particles and red blood cells, hemagglutination occurs.
- However, researchers may first mix a person’s serum with virions, followed by adding red blood cells. If no hemagglutination occurs, the serum antibodies have neutralized the measles viruses. Researchers consider this a positive test result for the presence of virus-specific antibodies.
- Researchers widely use hemagglutination inhibition tests to diagnose influenza, measles, mumps, mononucleosis, and other viral infections.
- The most routinely used techniques for identification of the mycoplasmas are hemagglutinin reactions, antigen-antibody reactions using the patient’s serum, and PCR.
- These microorganisms are slow growing; therefore, positive results from isolation procedures are rarely available before 30 days-a long delay that may put a patient’s life at risk.
- Researchers develop fungal serology to detect the serum antibody, but they limit it to very few fungi.
- Researchers use the cryptococcal latex antigen test for the direct detection of Cryptococcus neoformans.
- The clinical laboratory uses automated and non-automated methods for the rapid identification of yeasts.
- Any serological method used to detect fungi is best go with morphological studies examining for chlamydospores, pseudohyphae and yeast cell structure, and so on.
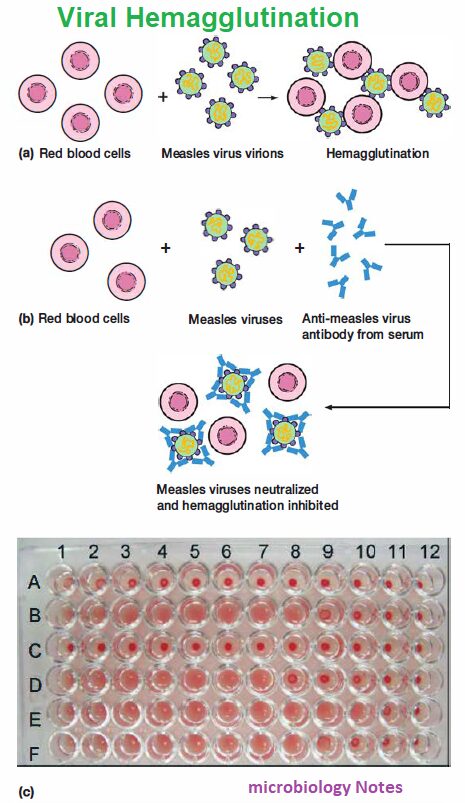
- Researchers also use agglutination tests to measure antibody titer.
- In tube or well agglutination tests, a technician adds a specific amount of antigen to a series of tubes or shallow wells in a microtiter plate.

- Researchers then add serial dilutions of serum (1/20, 1/40, 1/80, 1/160, etc.) containing the antibody to each tube or well.
- We determine the greatest dilution of serum showing an agglutination reaction, and the reciprocal of this dilution is the serum antibody titer.
Reference and Sources
- https://www.slideshare.net/chhaya30/diagnostic-microbiology
- https://laboratoryonline.blogspot.com/2010/11/
- https://microbiollogy.blogspot.com/2013/05/clinical-microbiology_23.html
- https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/antigen-antibody-reaction
- https://www.coursehero.com/file/11490467/Lec-20/
- https://lookformedical.com/en/search/hemagglutination-viral
Also Read:
- Bacterial Cell Walls
- Antibody or Immunoglobulin
- Nosocomial Infection: Introduction, Source, Control and prevention
- Polymerase Chain Reaction
- Virus: Introduction, Properties and Classifications
- Electrophoresis: Overview, Principles and Types
- Omicron: Overview, Transmissible, Vaccination and Severity of disease
- Immunoglobulin Classes: IgG, IgA, IgM, IgD and IgE
- Antigen-Antibody Reactions: Uses, Stages and Features