Introduction
- Hansen’s disease, also known as leprosy, is an ancient disease appearing throughout written history.
- Disfigurement, loss of limbs, and blindness can result from skin and peripheral nerve involvement.
- The number of new cases of Hansen’s disease has decreased dramatically since the introduction of multi-drug therapy; today it is most often seen in tropical or developing countries.
- Still, millions of people continue to suffer from the residual effects of their disease and the stigma associated with it.
- In the United States, about 100 cases are reported annually.
Signs and Symptoms of Hansen’s disease
- Hansen’s disease begins gradually, months or sometimes years after exposure.
- Onset is characterized by pigmentation changes and increased or decreased sensation in certain areas of skin.
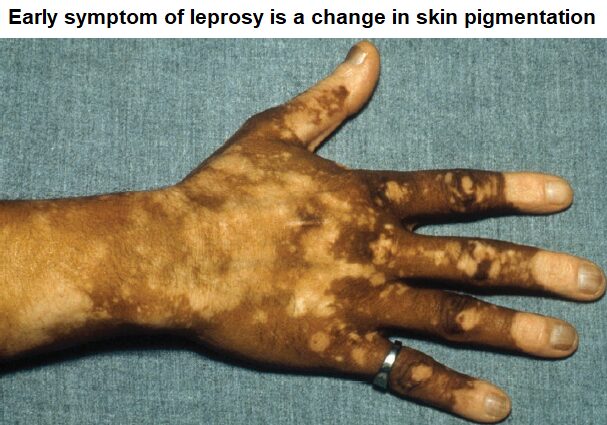
- These areas may thicken—losing hair, sweat glands, and all sensation.
- The nerves of the arms and legs may become visibly enlarged with accompanying pain, later changing to numbness.
- Loss of nerve activity can lead to muscle wasting, ulceration, and finally loss of fingers or toes due to unnoticed or untreated injury.
- In more severe cases, changes are most obvious in the face, with thickening of the nose and ears and deep wrinkling of the facial skin.
- Collapse of the supporting structure of the nose leads to congestion and bleeding.

Causative Agent of Hansen’s disease
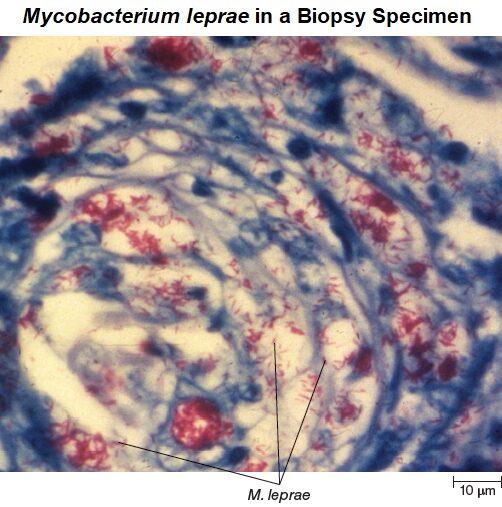
- Mycobacterium leprae is aerobic, rod-shaped, and acid-fast.
- It grows very slowly with a generation time of about 12 days, and prefers the slightly cooler temperatures of the body’s extremities.
- Hansen’s disease is usually diagnosed based on clinical findings, but skin biopsy specimens that show acid-fast rods can provide an early indication of nerve invasion.
- Despite many attempts, M. leprae has not been grown in the absence of living cells.
- It can, however, grow in the footpads of mice, in armadillos, and in mangabey monkeys.
- Moreover, a DNA library of M. leprae has been made and expressed in E. coli, providing large quantities of the organism’s antigens for study.
Pathogenesis of Hansen’s disease
- Mycobacterium leprae is the only known human pathogen that preferentially infects peripheral nerves.
- From there, the course of the infection depends on the immune response of the host.
- In most cases, cell-mediated immunity develops against the invading bacteria, and activated macrophages limit.
- The disease often spontaneously stops progressing, and the nerve damage, although permanent, does not worsen.
- This limited type of Hansen’s disease, in which cell-mediated immunity successfully stops the proliferating bacteria, is called tuberculoid leprosy (also called paucibacillary Hansen’s disease).
- People with tuberculoid leprosy rarely, if ever, transmit the disease to others.
- When cell-mediated immunity to M. leprae fails to develop or is suppressed, unrestricted growth of M. leprae occurs, leading to a form of Hansen’s disease called lepromatous leprosy (also called multibacillary Hansen’s disease).
- The bacteria first multiply in the cooler tissues of the body, notably in skin macrophages and peripheral nerves, and later throughout the body.
- The tissues and mucous membranes contain billions of M. leprae, but there is almost no inflammatory response to them.
- Mucus of the nose and throat contains high numbers of the pathogen, which can easily be transmitted to others.
Epidemiology of Hansen’s disease
- Transmission of Mycobacterium leprae is by direct human to human contact.
- The source of the organisms is mainly nasal secretions of lepromatous cases, which can transport M. leprae to mucous membranes or skin abrasions of other individuals.
- Even then, the disease develops in only a tiny minority, being controlled by immune defenses in the rest.
- Natural infections with M. leprae also occur in wild ninebanded armadillos, possibly due to their relatively low body temperature suitable for replication of the bacterium.
- Gene sequencing studies of animals in the southern United States confirm that the same strain of M. leprae is found in both humans and armadillos.
- Interaction with armadillos in these regions may explain cases of leprosy seen in individuals who have not traveled to a part of the world where the disease is considered endemic nor had contact with those who have.
- Eradication of Hansen’s disease, defined as less than 1 case per 10,000 individuals, has been achieved in most countries where the disease was endemic.
- It is difficult to completely eradicate, however, due to the long generation time of M. leprae.
- The long generation time results in an incubation period of about 3 years (range, 3 months to 20 years), during which time the disease can remain undetected.
Treatment and Prevention of Hansen’s disease
- Early treatment can keep Hansen’s disease from progressing.
- Since 1995, the World Health Organization has provided free multidrug therapy to patients, radically reducing the number of cases.
- Tuberculoid leprosy can be successfully treated by a combination of dapsone and rifampin administered for 6 months.
- Lepromatous leprosy is generally treated for a minimum of 2 years, with addition of a third drug, clofazimine, to the treatment process.
- Multiple drug therapy is required to prevent drug-resistant strains from developing.
- No proven vaccine to control Hansen’s disease is yet available.
Some features of Hansen’s disease are summarized in table
| Signs and symptoms | Skin lesions that lack sensation, deformed face, loss of fingers or toes |
| Incubation period | 3 months to 20 years; usually 3 years |
| Causative agent | Mycobacterium leprae, an acid-fast rod that has not been grown in the absence of living cells |
| Pathogenesis |
|
| Epidemiology | Direct contact with M. leprae from mucous membrane secretions. |
| Treatment and prevention | Treatment: Antimicrobial medication. Prevention: No vaccine. |
Reference and Sources
- https://healthjade.net/lepromatous-leprosy/
- https://en.wikipedia.org/wiki/Leprosy
- https://www.researchgate.net/publication/11019269_Leprosy_A_problem_solved_by_2000
- https://quizlet.com/279492025/bio105-exam-iii-resume-on-lecture-mon-312-flash-cards/
- https://quizlet.com/293935816/microbiology-final-exam-flash-cards/
- https://quizlet.com/31630694/chapter-26-flash-cards/
- https://quizlet.com/17662722/microbiology-final-flash-cards/
- https://www.nejm.org/doi/full/10.1056/NEJMoa1010536
- https://www.pnas.org/content/112/51/E7118
Also Read:
- SARS: Evolution of a Virus
- How to Build a Microorganism?
- Exposure and Transmission of Infectious Disease
- Gonorrhea: Causative Agent, Symptoms, Treatment and prevention
- Histoplasmosis: Symptoms, Pathogenesis, Treatment and prevention
- Cold sores : Introduction, Entry, Symptoms, Diagnosis and Cure
- Reverse Transcription Polymerase Chain Reaction (RT-PCR)
- Syphilis: Agent, Epidemiology, Symptoms, Treatment and Prevention
- Chlamydia: Introduction, Epidemiology, Transmission, Treatment and Prevention
- Microbiology Disciplines: Bacteria, Viruses, Fungi, Archaea and Protists

