Tissue Transplantation Rejection
Transplants between genetically different individuals within a species are termed allografts (Greek allos, other). Some transplanted tissues do not stimulate an immune response. For example, a transplanted cornea is rarely rejected because lymphocytes do not circulate into the anterior chamber of the eye. This site is considered an immunologically privileged site. Another example of a privileged tissue is the heart valve, which in fact can be transplanted from a pig to a human without stimulating an immune response. This type of grafts between different species is termed a xenograft.
Transplanting tissue that is not immunologically privileged generates the possibility that the recipient’s cells will recognize the donor’s tissues as foreign. This triggers the recipient’s immune mechanisms, which may destroy the donor tissue. Such a response is called tissue rejection. Tissue rejection can occur by two different mechanisms. First, foreign MHC molecules on transplanted tissue, or the “graft;’ are recognized by host T-helper cells, which aid cytotoxic T cells in graft destruction.

Cytotoxic T cells then recognize the graft because it bears foreign class I MHC molecules. This response is much like the activation of CTLs by virally infected host cells. A second mechanism involves the T-helper cells reacting to the graft and releasing cytokines. The cytokines stimulate macrophages to enter, accumulate within the graft, and destroy it. MHC molecules play a dominant role in tissue rejection reactions because of their unique association with the recognition system of T cells. Unlike antibodies, T cells cannot recognize or react directly with non-MHC molecules (viruses, allergens). They recognize these molecules only in association with, or complexed to, an MHC molecule.
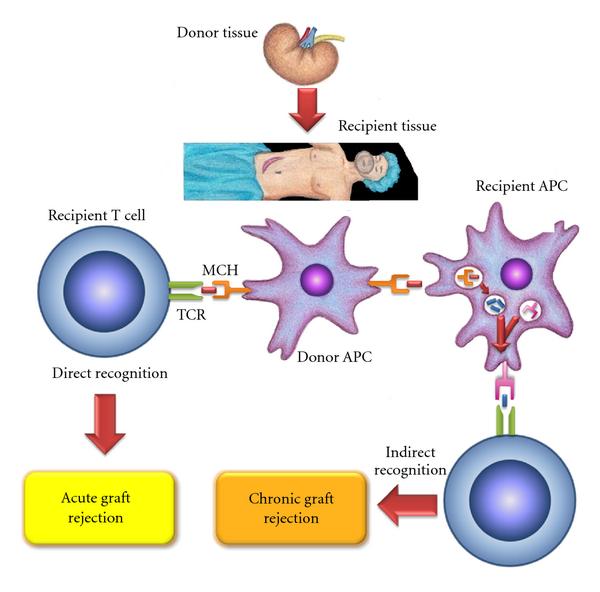
Because class I MHC molecules are present on every nucleated cell in the body, they are important targets of the rejection reaction. The greater the antigenic difference between class I molecules of the recipient and donor tissues, the more rapid and severe the rejection reaction is likely to be. Class II MHC molecule mismatch can also result in rejection and may be even more severe than class I mismatch reactions. However, the reaction can sometimes be minimized if recipient and donor tissues are matched as closely as possible. Most recipients are not 100% matched to their donors, so immuno suppressing drugs are used to prevent host mediated rejection of the graft.
Organ transplant recipients also can develop graft-versus host disease. This occurs when the transplanted tissue contains immune cells that recognize host antigens and attack the host. The immuno suppressed recipient cannot control the response of the grafted tissue. Graft-versus-host disease is a common problem in bone marrow transplants. The transplanted bone marrow contains many mature T cells. These cells recognize the host MHC antigens and attack the immunosuppressed recipient’s normal tissue cells.
Reference and Sources
- https://www.biologydiscussion.com/cell/immune-responses/cellular-immune-response-and-human-body-cellbiology/27257
- https://schoolbag.info/biology/microbiology/11.html
- https://quizlet.com/122584304/ap-ch16-flash-cards/
- https://quizlet.com/350783573/chapter-18-flash-cards/
Also Read:
- Hypersensitivity Reactions
- Granulocytes: Introduction, Types, Functions and Roles
- Animal and plant viruses, prions, and viroids
- Antimicrobial activity of Mimosa pudica l
- Bacteriophage: characteristics and replication of lytic and lysogenic cycle
- AIDS: Acquired Immune Deficiency Syndrome
- Cider: Production, Extraction, Fermentation and Maturation
- DNA Replication in eukaryotes: Initiation, Elongation and Termination
- Microbial Fuel Cells
