Fungal Diseases of Hair, Skin, and Nails
Introduction
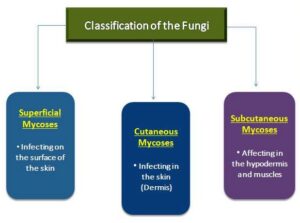
- Mycoses are referred to as fungal diseases, and classified according to the site of infection which is as follows:
- Superficial Mycoses
- Cutaneous Mycoses
- Subcutaneous Mycoses
- Mycoses also affects numerous systems of our body, e.g., it can cause lung infections, blood infections & meningitis.
- Even mycoses affecting organs or blood of the human body can also cause secondary infection on the skin.
- Fungi can only affect when their growth is favorable and the host immunity is compromised.
- Usually, both superficial & cutaneous mycose affects nails, skin, and hair, not considered fatal but are recurring and not easy to get rid off.
Superficial Mycoses
- The most generally occurring fungal infections are restricted to the hair, nails, and surface of the skin.
- The epidermal layer is made up of keratin & dead cells.
- Surface infection by opportunistic mycoses occurs by direct contact with its spores or hyphae.
- E.g., Pityriasis
Signs and Symptoms
- Pityriasis versicolor (because of variable skin pigmentation), characterization is done by the appearance of the scaly skin which has hyperpigmentation or hypopigmentation patches.

- Mycose interferes with the production of melanin, usually occurs on the arms, trunk, and shoulders, rarely on the neck or face.
Pathogens & Virulence Factors
- The causative agent of Pityriasis versicolor, is a basidiomycete, Malassezia furfur which are dimorphic (exist in two forms, hyphae and yeast).
- It gains nutrition from sebum produces by the skin, tends to be recurring.
Epidemiology & Pathogenesis
- Superficial mycoses produce an enzyme, keratinase which breaks down the keratin.
- It usually doesn’t penetrate the tissues helps them to cause the disease on the skin surface because the immunity of the host is not triggered.
- Transmission is carried by fungal spores or hyphae on the surface of the personal use items, mostly hairbrushes, and combs, which can cause spread in the group of members like in family if the item is shared.
- Most susceptible are adolescents, because of increased production of sebum due to hormonal change and also in immuno compromised patients, even it can do worse like evading in the deeper tissues and cause systemic infections.
Diagnosis & Treatment
- A quick examination can be done by using UV illumination (at the wavelength of 365nm), its fluorescence is pale green color.
- Definitive diagnosis can be carried by microscopic examinations, slide preparation is done by using affected skin sample mixed with 10% of KOH, on observation both hyphal form & budding yeast can be seen.
- Treatment: Topical solutions of antifungal imidazole for e.g., ketoconazole shampoos, or ciclopirox, other topical solutions such as selenium sulfide lotions, zinc pyrithione, or propylene glycol can be used.
- To treat rigid infections, which fail to respond to topical medications, oral therapy such as ketoconazole is required.
- Prophylactic topical treatment is needed because of the reoccurrence of the disease.
- The pigmented or hypopigmented skin takes months to regain its normal color.
Cutaneous Mycoses
- Few fungi, cause cutaneous lesions known as dermatophytoses, causative fungi are known as dermatophytes.
- Growth occurs on skin, hair, and nails, which can invade the body.
- It stimulates cell-mediated immune response which can destruct the tissue (deeper level).
Sign & Symptoms
- Previously, it was called ringworms, or tinea because of their appearance that was scaly patches on the skin.
- Both ringworms and dermatophytes are misnomers because no worms are involved & phytes refer to the plants.
- The common form of dermatophytosis. is the Athlete’s foot.

Common Fungal Species causing Dermatophytosis
- Usually, ascomycetes are responsible for fungal infection in the cutaneous mycose:
- Microsporum
- Trichophyton
- Epidermophyton floccosum
- All three are responsible for infections on skin & nails, Trichophyton also infects the hair scalp.
Table: Common Forms of Dermatophytosis
| Disease | Fungi Involved | Common Signs | Source |
| Tinea capitis | Microsporum canis Microsporum gypseum Trichophyton equinum Trichophyton verrucosum Trichophyton tonsurans Trichophyton violaceum Trichophyton schoenleinii |
|
Humans (contact with contaminated soil or animals) |
| Tinea corporis | Trichophyton rubrum
Microsporum gypseum Microsporum canis |
|
Can spread from other body sites (contact with contaminated soil or animals) |
| Tinea unguium (onychomycosis) |
Trichophyton rubrum;
Trichophyton mentagrophytes var. interdigitale |
|
Humans |
| Tinea cruris (“jock itch”) |
Trichophyton rubrum
Trichophyton mentagrophytes var. Epidermophyton floccosum |
|
Usually spreads from the feet |
| Tinea pedis (“athlete’s foot”) |
Trichophyton rubrum
Trichophyton mentagrophytes Epidermophyton |
|
Human reservoirs in the toe webbing; carpeting holding infected skin cells |
Pathogenesis
- Keratin is a source of nutrition for these opportunistic fungi, they colonize the surface of the skin, hair, and nails.
- It triggers the cell-mediated immune response, which also damages the living cells.
- These mycoses both subcutaneous & cutaneous ones, grow on dead decaying organic matters on the soils when its spores or hyphae come in contact with the skin, when conditions are favorable it grows and invades the deeper tissues (dermis or hypodermis).
Epidemiology
- It is a contagious disease because infected individual sheds dead skin cells, & hairs including fungal spores & hyphal elements, and its reoccurs even it’s treated.
- Classification of Dermophytes infecting humans is done on the basis of the natural niches:
- Anthropophilic dermatophytes: Spread by close contact with an infected individual, related to humans only.
- Zoophilic dermatophytes: Spread by pets or animals to humans, or even contaminated animal products such as wool.
- Geophilic dermatophytes: Present in soil, only spread by direct exposure of humans through soils.
Diagnosis & Treatment:
- Clinical observation is generally enough to diagnose infections because of their symptoms.
- Definitive diagnosis: It is done by microscopic examinations, the slide is prepared with infected skin, nail or hair scraping, and potassium hydroxide (KOH) 10%, it can reveal the hyphae or conidia (asexual spores) of the fungi.
- Treatment:
- Topical antifungal agents are used, but when widespread infections on nails, skin, and hairs occur, oral antifungal agents are preferred.
- Terbinafine is used as an antifungal topical agent, for effective results, it is used for 3-4 weeks.
- For chronic or recurrent cases, Griseofulvin is used.
Subcutaneous or Wound Mycoses
- Some fungi invade deeper tissues of the human body, i.e., bone and hypodermis (doesn’t become systemic).
- Initially, it grows on the epidermis of the skin and produces lesions on the surface.
- The wound mycoses are as follows:
- Chromoblastomycosis
- Phaeohyphomycosis
- Mycetoma
- Sporotrichosis
| Disease | Fungi Involved | Common Signs | Diagnosis | Treatments |
| Chromoblastomycosis | Fonsecaea pedrosoi
Fonsecaea compacta Phialophora verrucosa Cladophialophora carrionii |
Appears as small, itchy but painless, scaly lesions on the skin. it becomes tumorlikeInflammation, development of fibrous tissue, and abscess formation |
Microscopic examination of stained skin scrapings (golden brown bodies – key features),
Macroscopic examination of colonies Microscopic examination of spores |
Difficult to treat (extreme cases)
Earlier Extensive lesions may require amputation- along with a prolonged course of thiabendazole and 5-fluorocytosine |
| Phaeohyphomycosis | Alternaria
Exophiala Wangiella Cladophialophora |
Paranasal sinus phaeohyphomycosis: colonization in the nasal passages (cause allergy-like symptoms).In cerebral phaeohyphomycosis, the brain is involved ( RARE) |
Stained skin scrapings, biopsy material, or cerebrospinal fluid (CSF)- microscopic observation (Brown-pigmented hyphae is seen) | Itraconazole |
| Mycetomas | Madurella
Pseudallescheria Exophiala Acremonium |
Small, hard, subsurface nodules are formed
Local swelling, ulcerated lesions (with pus) Infected areas have oily fluid ( fungal spores & hyphae is present) |
Symptoms and microscopic demonstration of fungi helps in diagnosis | Surgical removal
Amputation Ketoconazole |
| Sporotrichosis (Rose gardener’s disease) |
Sporothrix schenckii | Fixed sporotrichosis: Nodular lesions at infected site, pus-filled dischargeLymphocutaneous sporotrichosis: Primary & Secondary lesions is formed |
Pus or biopsy tissue is stained using silver – Microscopic observation | Topical applications of saturated KI for several months. Itraconazole & amphotericin B |
References and Sources
- https://quizlet.com/201583675/microbiology-with-disease-by-body-system-chapter-19-disease-of-the-skinand-
wounds-flash-cards/ - https://www.infectiousdiseaseadvisor.com/home/decision-support-in-medicine/infectiousdiseases/
superficial-mycoses-dermatophytosis/ - https://www.researchgate.net/publication/50410768_Spectrum_of_Mycoses
- https://quizlet.com/515478627/ch-19-microbial-diseases-of-the-skin-and-wounds-flash-cards/
- https://people.wou.edu/~guralnl/gural/318fungi.pdf
- https://quizlet.com/40856019/micro-chapter-19-flash-cards/
- https://verheiratetbusdrinnen.com/cdi/selsun-blue-salonlc3r3412i-7t0.html
- https://www.researchgate.net/publication/276839856_Antifungal_Treatment_for_Pityriasis_Versicolor
- https://onderwegkeinem.com/k4a-63787v7q5se/Seborrheic-dermatitis-scalp-treatment.html
Also Read:
- Fungal Disease
- Introduction of Plant-Microbe Association and the Mycorrhizae
- Pseudomonas aeruginosa-Etiology, Pathogenesis and Treatment
- Leishmaniasis- Epidemiology, Clinical symptoms and Treatment
- Normal Microbiota of the Healthy Human body
- Staphylococcus aureus-Epidemiology, Pathogenesis & Treatment
- Methods for Laboratory diagnosis of viral infections
- Fungi: Distribution, Morphology, Reproduction, Classification
