Introduction
Antimicrobial chemotherapy refers to the use of chemical substances to kill or inhibit the growth of microorganisms such as bacteria, fungi, protozoa, and viruses that cause infectious diseases. These chemical agents are called antimicrobials and include antibiotics, antifungals, antivirals, and antiparasitic drugs.
- Usually, the pathogen causes infection in human hosts, to eradicate them, chemotherapeutic agents such as antibiotics are used.
- Its action requires inhibiting or killing of pathogen while causing less harm to the host.
- Different antimicrobial compounds have a variety of effects on the pathogens such as:
- Disruption of structure or process involves infection by pathogens.
- Interferes in the synthesis of cell wall.
- Inhibits synthesis of a protein or nucleic acid.
- By blocking enzymes or metabolic pathway involves in infection.
- Chemotherapeutic agents are generally used as modern medicine to deal with infections.
- These are basically chemical agents, it may be derived from microbial sources such as bacteria and fungi or can be synthesized synthetically, agents are termed antibiotics.
- For e.g microbial derivative antibiotics are penicillin obtained from penicillium, and chemically synthesized antibiotics are sulfonamides.

Historical Development of Chemotherapeutic agents
- Paul Ehrlich, in 1854–1915, purposed a “magic bullet“, one of the dyes that could selectively destroy pathogens causing infection in the human host.
- In 1904, he found dye trypan red was effective against the trypanosome, which causes sleeping sickness and can be used for its treatment.
- Sahachiro Hata found out arsphenamine was effective against syphilis caused by a spirochete, commercially it was launched by the name called Salvarsan.
- Gerhard Domagk screened more chemicals for similar results like magic bullets.
- He found Prontosil Red, a dye used for staining leather, has effective results against Staphylococci and Streptococci infections.
- Jacques and Therese Trefouel discovered sulfonamides or sulfa drugs and explained body metabolizes the dye to sulfanilamide.
- Alexander Fleming, in the 1920s, discovered penicillin obtained by Penicillium notatum, which was the first true antibiotic for therapeutic uses.
- Howard Florey, in 1939, studied the bactericidal activity of several substances, such as sulfonamides and lysozymes.
- Further studies on penicillin, its production, and purification were carried out by Ernest Chain and Florey.
- The Nobel Prize was awarded to Fleming, Ernest Chain, and Florey in 1945 for the discovery and production of penicillin.
- Selman Waksman in 1944, discovered streptomycin obtained from Streptomyces griseus.
- More discovery and development of antibiotic compounds cause a revolution in the treatment of human diseases.
What characteristics are needed for effective antimicrobial drugs?
- Selective Toxicity- Chemotherapeutic drugs, are selectively toxic to pathogens and cause less harm to the human hosts.
- It depends on the following factors:
- Therapeutic dose– level of drugs requires for treatment.
- Toxic dose– The level of drug which is toxic to the host, is measured in terms of therapeutic index, and it’s a ratio of the therapeutic dose to the toxic dose. [Effective chemotherapeutic drugs have a higher therapeutic index].
- The less therapeutic index of drugs causes many side effects in the host.
- A drug that offers selectively toxicity mainly disrupts microbial function which is absent in eukaryotic cells.
- For instance, penicillin acts by inhibiting the synthesis of peptidoglycan, which is a component of the bacterial cell wall, and host cell lack cell wall, therefore antibiotics have less effect on it.
- Range of effectiveness – broadly defined into two categories:
- Narrow-spectrum drug- Effective on a limited variety of microorganisms.
- Broad- Spectrum drugs- Effective on a broad range of microorganisms.
- Semisynthetic drugs have a high range of effectiveness, it is obtained from a natural source and the chemical group is added for structural modification of drug. E.g., Amoxycillin and ampicillin.
- Classification of the drug is done by action on the particular microbial group- Antibacterial, Antiviral, Antifungal and Antiprotozoan.
- The action of the chemotherapeutic drug can be static or cidal; static agents inhibit the growth, it’s more effective when a host resistance mechanism is high, in absence of an agent, microorganisms reversibly grow. Cidal agents kill the target microorganisms.
- The nature of the drug is concentration-dependent, i.e., at low concentration, it may act as static and at high, it may have cidal effect on the pathogen.
- The effect of drugs varies on target microorganisms, in some pathogens drugs may act cidal whereas in other pathogens they may act as static agents.
How the effectiveness of the drug is measured?
There are certain tests that are carried out to determine the effectiveness of the drug on the target pathogen which are as followed:
Dilution Susceptibility Tests
- Used to calculate the values of minimal inhibitory concentration (MIC), which is the minimum concentration of drug to prevent microbial growth, and minimal lethal concentration (MLC), the minimum concentration of drug which is capable to kill target pathogen.
- These dilution tests can be performed in both broth and agars.
- For broth dilution test, Mueller- Hinton broths with a range of antibiotic concentration from 0.1 to 128 µg/ ml are prepared.
- The standard test organism is inoculated in the broths.
- The broth containing a minimum concentration of the antibiotic shows no growth after 16- 20 hrs is considered as MIC value.
- The MLC value can be determined by the minimum concentration of antibiotics from which microorganisms don’t grow in the broth even when it’s transferred in a fresh medium without antibiotics.
- In the agar dilution test, Mueller- Hinton agar mediums with different ranges of antibiotics are inoculated and examination is done the same as broth dilution test.
- An automated system for the determination of MIC is currently used.
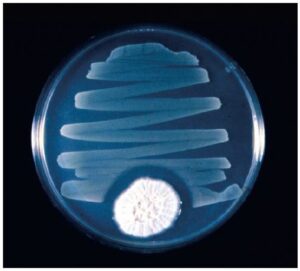
Disk Diffusion Tests
- The principle used in this method is antibiotic- discs are placed on the agar medium which slowly diffuses outward and forms a clear zone indicating no growth around the disc, size of the zone depends on the concentration of antibiotic diffused.
- Kirby-Bauer method is a commonly used disk diffusion test developed by William Kirby and A.W. Bauer.
- Pathogen or test microorganisms are cultured in the broth and incubated for a few hrs at 35°C
- A cotton swab is dipped in the culture broth and spread evenly on Mueller- Hinton agar medium
- Antibiotic disks are placed on an agar medium with a sterilized forceps.
- Incubated it for 16- 18 hrs at 35°C, clear zones diameter is measured.
- Result interpretation – If microorganism sensitivity to the drug, its MIC value decreases and zone of inhibition is larger whereas microorganism’s resistance to the drug, Its MIC increases and zone of inhibition is small.

The Etest
- It is used to test antibiotic sensitivity in anaerobic pathogens.
- An agar medium is streaked with a target pathogen and plastic Etest strips are placed on the surface of the agar.
- Each Etest strip is labeled with Mic values and contains gradients of antibiotic, the lowest concentration in the strip is placed in the center of the medium.
- After incubation up to 24-48 hrs, a zone of inhibition in elliptical shape is observed.

Reference and Sources
- https://themicrobialworld.wordpress.com/lecture-notes/chapter-7/
- https://www.researchgate.net/publication/317307215_Classification_of_Anti-Bacterial_Agents_and_Their_Functions
- https://courses.lumenlearning.com/trident-boundless-microbiology/chapter/overview-of-antimicrobialtherapy/
- https://openstax.org/books/microbiology/pages/14-3-mechanisms-of-antibacterial-drugs
- https://phdessay.com/lab-report-antibiotic-evaluation-by-the-kirby-bauer-method/
- https://www.researchgate.net/publication/286280523_Enzymatic_structural_modification_of_natural_products

