Mycobacterium tuberculosis-Epidemiology, Pathogenesis, and Treatment
Introduction
- M. tuberculosis is gram-positive rods, aerobic, non-motile, non-spore-forming, intracellular bacteria.
- It has fastidious growth requirements, growth is enhanced by CO2 (5%-10%), divides slowly (up to 8 weeks), because of the complex cell wall.
- The common culture medium is Lowenstein- Jensen (composed with homogenized egg in the base nutrient), colonies appear after 3-6 weeks, they are rough, dry & light brownish yellow color colonies.
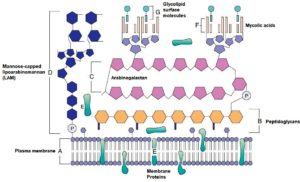
- Cell Structure – It is rich in lipids, with hydrophobic exteriors which provide resistance against various disinfectants, stains, acids & alkalis.
- It is different from a typical gram-positive cell wall structure :
- In the plasma membranes, phosphatidylinositol mannosidises, proteins, and lipoarabinomannan (LAM) are anchored.
- LAM has a functional association with the O-antigenic lipopolysaccharide that exists in bacteria.
- Porins and Transport protein span across the cell wall.
- The proteins have biological significant antigens, triggers the host’s cellular immune response, also used for diagnosis purposes as purified protein derivatives (PPDs).
Pathogenesis
- M. tuberculosis can cause lifelong infection, it affects the respiratory tract.
- When exposed, M. tuberculosis enters the respiratory airways & penetrates the alveoli, gets phagocytosed by alveolar macrophages.
- Bacteria prevents phagosome fusions with lysosomes (by blocking early endosomal autoantigen 1(EEA1).
- Instead phagosome fuse with intracellular vesicles (permit access to nutrients & replication).
- Macrophage secretes interleukin-12(IL-12) & tumor necrosis factor-α (TNF-α), in response to the infection.
- Cytokines increasing localized inflammation ( recruits T cells, NK cells, required interferons)
- People who have decreased productions of cytokines (IL-12 & TNF-α) or defects in cytokines receptors are at major risk of mycobacterial infections.
- Fused macrophages / Langhans giant cells/epithelial cells, with mycobacterium, form a necrotic mass (present in core) surrounded by a thick wall of macrophages & NK T cells, CD4 & CD8 which is completely called a granuloma.
- It prevents the further spread of the infection.
- Less antigenic burden leads to the formation of the small granuloma with minimal tissue damage.
- More bacteria are present, large necrotic granulomas are formed, encapsulated within fibrins which provide resistance against macrophage killing. (Bacteria can remain in a dormant stage and reinfect when the host immune system is weakened (old age or disease- called Reactivation).
Epidemiology
- The natural reservoirs are humans and primates.
- The mode of transmission is by person-to-person contact (by inhaling infectious droplets).
- According to WHO, 1/3 rd of the population is infected by the disease tuberculosis.
- The mortality rate per year is 2 million / yr and new cases are 9 million worldwide.
- The highest incidence includes regions such as sub-Saharan Africa, Eastern Europe & Southeast Asia.
- People susceptible to disease caused by M.tuberculosis are drug & alcohol abusers, HIV patients, also health care workers.
Sign & Symptoms
- The primary infection of tuberculosis is majorly asymptomatic or clinical symptoms like fever & malaise occur.
- The infiltrates in the lung (mid-zone) & enlarged lymph nodes can be observed by radiographs. It occurs in Pulmonary tuberculosis.
- The symptoms include dry cough (main), as a disease progresses there is sputum production, mixed with blood (known as hemoptysis), fever, sweating, malaise, fatigue, & weight loss comes along with the further disease progression
- The disease can also involve other organs such as bone, kidneys, brain, meninges & bowel.
- The untreated progressive disease usually takes 2-5 yrs to cause death but is rapid in HIV or immunocompromised patients.
Diagnosis
- A very common diagnostic test to find out the exposure to the organism is the Tuberculin test (test for PPD) & Interferon -γ release, these are sensitive markers.
- Detection can be done by using microscopic observation of clinical specimens (sputum) smeared with Ziehl- Neelsen procedure.

- Molecular probes are quite helpful in the diagnostic procedure.
Treatment
- M. tuberculosis is susceptible to various effective antimicrobial agents as follows:
First Line Drug |
Second Line Drug |
| Isoniazid (Disrupts mycolic acid) | Para-Aminosalicylic acid |
| Ethambutol (affects LAM element in the cell wall) | Ethionamide |
| Rifampin | Cycloserine |
| Pyrazinamide | Fluoroquinolones (e.g., ciprofloxacin & ofloxacin) |
| Streptomycin (Inhibits cell wall synthesis) | Kanamycin |
- Second lines drugs are used in combinations with the first lines drugs if resistance or toxicity prevails.
- The oral chemotherapy treatment (Isoniazid & Ethambutol) of the disease, is usually continued for 18- 24 months.
- The time period of treatment is shortened by 6 months by using isoniazid, rifampin & pyrazinamide.
- For prevention, the BCG vaccine (Bacillus Calmette-Guerin) is available.
References & Sources
- https://quizlet.com/155098300/mmi-unit-3-flash-cards/
- https://www.researchgate.net/publication/8666585_Tuberculosis_A_problem_with_persistence
- https://quizlet.com/57381644/pathogenic-microbiology-test-3-note-cards-flash-cards/
- https://www.sciencedirect.com/topics/medicine-and-dentistry/blue-rubber-bleb-nevus-syndrome
Also Read:
- Phagocytosis-Introduction and Mechanisms
- Second Golden Age of Microbiology
- Bacteria: Shape, Size, Structure and other Membrane
- Algae : occurrence, classification and economic importance
- Hansen’s Disease: Symptoms, Causative Agent, Pathogenesis and Treatment
- Pseudomonas aeruginosa-Etiology, Pathogenesis and Treatment
- Shigella-Epidemiology, Pathogenesis, and Treatment
- Normal Microbiota of the Healthy Human body
