Introduction
- Antibiotics can damage pathogens in different ways.
- Mode of actions varies in different antibacterial drugs or antibiotics.
Generally, they affect the machinery of pathogens such as:
-
- Inhibits the cell wall synthesis.
- Inhibits synthesis of protein.
- Inhibits synthesis of nucleic acid.
- Metabolic antagonists.
Inhibitors of Cell Wall Synthesis
- Antibiotics such as penicillins, cephalosporins, vancomycin, and bacitracin interfere with the synthesis of the cell walls.
- The therapeutic index of these antibiotics is high, as it is selectively toxic to target pathogens.
Penicillins
- Many types of penicillins are derivatives of 6-aminopenicillanic acid consist of lactam ring and differ with respect to their side chains attached to their NH2 group.
- Many penicillin-resistant bacteria produce the enzyme penicillinase or lactamase, which hydrolyses the lactam ring and inactivates the antibiotic.
Mechanism of Penicillin
- It has structural similarity with peptidoglycan subunit blocks the catalysis of enzyme which is involved in transpeptidation reaction, which works to forms cross-linking of peptidoglycan.
- Block the complete formation of the cell wall, which causes osmotic lysis.
- Works only on growing bacteria that are still in process of synthesizing new peptidoglycan.
- Interact with several periplasmic proteins, which activate the autolytic enzymes of the target bacteria
- May activate a special protein named bacterial holins, which create holes and lesions in the membranes, which cause membrane leakage and eventually death.
- Additionally, murein hydrolases can come into action and destroy cells much more effectively, they move through holes, cause disruption in the peptidoglycan, and cause cell lysis.
Penicillin G – It is effective against gram-positive pathogens such as Staphylococci & Streptococci, administered by the parenteral route because it is disrupted by acid produced in the stomach whereas penicillin V can be consumed orally.
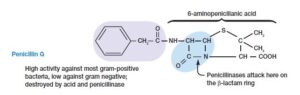
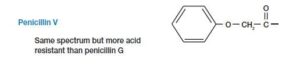
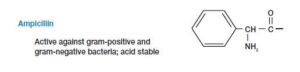
Ampicillin is potent on gram-negative bacteria e.g., Salmonella, Shigella, and Haemophilus.
Carbenicillin and Ticarcillin are effective against Pseudomonas and Proteus.


- Pathogens are becoming resistant against natural and semisynthetic penicillin, to cope up with this problem, specific semisynthetic penicillins such as methicillin, nafcillin, and oxacillin, are used. These antibiotics are not destroyed by lactamase.

- The rising cases of new resistance bacteria against antibiotics are a serious concern, which can cause the ineffectiveness of drugs against pathogens.
Cephalosporins
- It is obtained from the fungus Cephalosporium in 1948,
- Mechanism of Cephalosporins is alike to penicillin i.e., to inhibit the formation of the cell wall by blocking enzyme for cross-linking of peptidoglycan
- For patients who experience penicillin allergy, cephalosporin is used for treatment.
- Cephalosporin is a broad-spectrum drug, broadly classified into four generations as it was sequentially developed.
- First Generation i.e., effective against gram positives.
- The second generation is a modified version of first-generation, which has better effects on the gram –ve bacterias and some anaerobic bacteria.
- The third generation is effective against gram –ve pathogens and some drugs can reach CNS.
- Fourth-generation provides broad-spectrum coverage against gram-positive and negative, effective on Pseudomonas aeruginosa, which is considered as difficult opportunistic pathogens.



Vancomycin & Teicoplanin
- Vancomycin is produced by Streptomyces orieintalis.
- It is a glycopeptide antibiotic, composed of peptides linked to disaccharides.
- Mechanism – Specifically binds to terminal sequence on pentapeptide region of peptidoglycan which blocks the transpeptidase reaction.
- Effective against Bacillus, Streptococcus, and Clostridium
- Can be given intravenously or orally.
- Teicoplanin is obtained from actinomycetes Actinoplanes teichomyceticus, act similarly as vancomycin, potent on gram-positive bacteria which include Staphylococci, Streptococci, Clostridia, Enterococci, and Listeria
Inhibitors of synthesis of Protein
- Most antibiotics interact with ribosomes in prokaryotes, stops the synthesis of proteins.
- The therapeutic index of the drug is high, therefore can differentiate between ribosomes of prokaryotes and eukaryotes.
- There are several steps in the synthesis of the protein, that are hampered by the action of a drug, while some bind to the small subunit of ribosome 30S and others bind to large subunits 50S.
Aminoglycosides
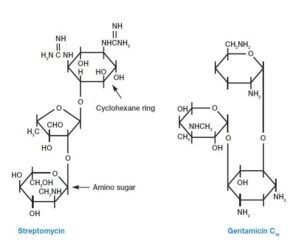
- There are several modifications in the aminoglycoside structure of the antibacterial drugs, which usually contain cyclohexane rings & amino sugars.
- It includes kanamycin, streptomycin, neomycin, & tobramycin synthesized by various species of Streptomyces, and gentamicin is synthesized by actinomycetes, Micromonospora purpurea.
- They are bactericidal in nature
- Streptomycin is used to treat tuberculosis and plague, its usage is reduced because of rising cases of streptomycin drug resistance.
- Gentamicin is generally used to treat infections caused by Proteus, E.Coli, Klebsiella, & Serratia.
- Aminoglycosides antibiotics cause more side effects and can cause serious damage to the host such as deafness, renal failure, nausea, allergic responses.
Tetracyclines
- It belongs to the group of antibiotics, which consists of a four-ring structure; the side chain is attached with side chains that vary in different modified tetracyclines.
- Naturally produced tetracyclines such as oxytetracycline & chlortetracycline were obtained from Streptomyces.
- Mechanism- It binds with 30S small ribosomal subunit that inhibits A- site binding with aminoacyl-tRNA molecule.
- This drug is bacteriostatic in nature.
- It is considered a broad-spectrum drug, it is usually potent on gram-negative and gram-positive and also rickettsias, mycoplasma, and chlamydiae.
- High doses of drugs result in diarrhea, nausea, and yellowing of teeth in children, it also causes damage to the liver and kidney.
- Tetracyclines are used in acne treatment other than that it is rarely preferred.

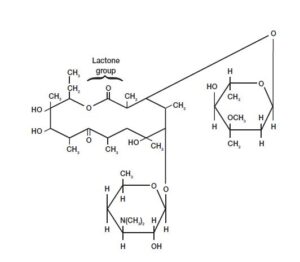
Macrolides
- It contains 12- 22 C lactone rings linked with sugars.
- Erythromycin, interact with 23 rRNA of the large subunit of ribosome 50S, to inhibits elongation of peptide chain during synthesis of the protein.
- This drug has a bacteriostatic effect on the pathogen.
- It is considered a broad-spectrum drug, potent on gram-positive bacteria and some gram-negative bacteria.
- Used to treat diphtheria, whooping cough and diarrhea [by Campylobacter], and also pneumonia caused by Mycoplasma & Legionella.
- Azithromycin is used for treatment caused by Chlamydia trachomatis.
- Other macrolide antibiotic is Clindamycin, effective against various bacteria including Staphylococcus and Bacteroides.
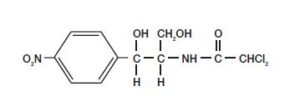
Chloramphenicol
- It was first obtained from Streptomyces venezuelae, now manufactured chemically.
- Mechanism- It binds to 23 S rRNA on a large subunit of ribosome 50S, inhibiting the reaction carried out by peptidyl transferase.
- It is a broad-spectrum drug but it is toxic, as it causes allergic responses or neurotoxic reactions.
- The most common adverse effect is aplastic anemia [in this condition formation of new blood cells is disabled] and a decrease in the number of WBC.
Inhibiting the Nucleic acid Synthesis
- Some antibacterial drugs disrupt nucleic acid synthesis by interfering with enzymes, such as DNA helicase, DNA polymerase, & RNA polymerase which eventually block DNA replication & transcription.
- These drugs are not selectively toxic, because nucleic acid synthesis doesn’t have a great difference between eukaryotes and prokaryotes.
Quinolones
- It contains 4- quinolone rings in their structure, used to hamper the synthesis of nucleic acid, and have a bactericidal effect on the pathogen.
- In 1962, the first quinolone, nalidixic acid was produced; currently, ciprofloxacin, norfloxacin & ofloxacin are commercially used.
- Mechanism- it inhibits two essential enzymes, DNA gyrase [used to separate DNA strand by introducing negative twist] & topoisomerase II [untangle DNA during DNA replication] which plays a significant role in DNA replication, eventually ceases DNA replication and its repair.
- It is considered a broad-spectrum antibiotic.
- It is particularly potent against enteric bacteria which include E.Coli, Klebsiella and also affects gram-negative and gram-positive pathogens which include Staphylococcus aureus, Mycobacterium tuberculosis.
- It is also used in the treatment of infection of the urinary tract, respiratory, skin, gastrointestinal, and sexually transmitted diseases [STD].
- The adverse effects of drugs are diverse but gastrointestinal upset is most common.

Metabolic Antagonists
- It acts as antimetabolites, by competitive inhibition of substrate i.e., metabolites, drug block or antagonize metabolic pathways
- Mechanism- It acts as a structural analog to the natural intermediates of metabolic pathways.
- Have a bacteriostatic effect on pathogens, and are considered broad-spectrum drugs.
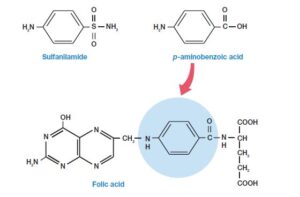
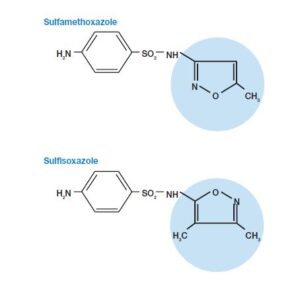
Sulfonamides
- Sulfonamides, discovered by G.Domagk, were used as chemotherapeutic agents as first antimetabolites.
- They are structurally analogous to p-aminobenzoic acid [PABA], which is used in the formation of the folic acid.
- Mechanism- For active sites of an enzyme drug competes with PABA, which hampers the synthesis of purines and pyrimidine. Therefore bacteria die, as their DNA replication ceases.
- This drug therapeutic index is high since bacteria synthesize their own folate whereas humans acquire it from the diet.
- Some patients experience side effects, such as allergic response which includes high fever, rashes.
Trimethoprim
- It’s a synthetic antibiotic, inhibits the synthesis of folic acid.
- Mechanism- It includes binding to the enzyme, dihydrofolate reductase (DHFR) which converts dihydrofolic acid into tetrahydrofolic acid, which competes against the substrate of dihydrofolic acid.
- It covers a broad-spectrum range of pathogen.
- It is used to treat infections of the respiratory, middle ear, urinary tract, and traveler’s diarrhea.
- To increase the efficiency of trimethoprim, usually used in combination with sulfa drugs to block folic acid synthesis.
- The common adverse effects a person experiences are loss of appetite, vomiting, abdominal pain, and tongue swelling, to reduce side effects it’s taken after food intake.

Reference and Sources
- https://biologywriteup.blogspot.com/2014/10/control-of-microbial-growth-bacterial.html
- https://www.scribd.com/document/490400369/Biology-10
- https://quizlet.com/200075652/chapter-20-flash-cards/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2896384/
- https://bio.libretexts.org/Courses/Portland_Community_College/Cascade_Microbiology/17%3A_Antimicrobial_Drugs/17.3%3A_Antibacterial_Drugs
- https://en.wikipedia.org/wiki/Peniciline
- https://microbiologyjournal.org/molecular-characterization-of-quinolone-resistant-urinary-isolates-ofescherichia-coli/
- https://www.chegg.com/homework-help/questions-and-answers/concept-selective-toxicity-relatestherapeutic-index-antibiotics-antibiotics-considered-go-q55218056
Also Read:
- Antiviral Drugs
- Anti protozoan Drugs
- Tetanus – Etiology, Pathogenesis, and Treatment
- Membrane Structure, Its Related Proteins and Hydropathy Plot
- Tetanus – Etiology, Pathogenesis, and Treatment
- Antimicrobial Chemotherapy: History, Characteristics and Tests
- Normal Microbiota of the Healthy Human body

